For parents with a baby in the NICU, hearing that your child may need a tracheostomy can feel overwhelming. This guide will walk you through what a tracheostomy is, why it’s sometimes needed, and how families can prepare for life after the NICU with a tracheostomy tube, or a “trach”.
What Is a Tracheostomy?
A tracheostomy (pronounced tray-kee-OS-tuh-mee) is a surgical procedure that creates a small opening in the baby’s neck directly into the windpipe (trachea). A short tube called a tracheostomy tube or “trach” is placed into this opening to help your baby breathe.
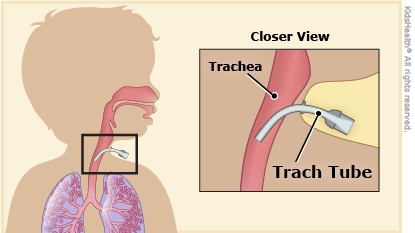
In some babies, breathing through the nose or mouth isn’t possible or safe due to long-term ventilation needs, airway obstruction, or abnormal airway anatomy. A tracheostomy provides a more stable, long-term way to support breathing.
Why Might a Baby in the NICU Need a Tracheostomy?
Tracheostomies are typically considered when other options like intubation (a breathing tube through the mouth or nose) are no longer ideal or safe. Common reasons include:
- Long-term ventilation: Babies who need a ventilator for many weeks or months due to chronic lung disease, severe prematurity, or neuromuscular weakness.
- Airway obstruction: Conditions that narrow or block the upper airway, such as laryngomalacia, subglottic stenosis, vocal cord paralysis, or craniofacial anomalies.
- Neurological conditions: Infants with certain brain or nerve disorders may not have a strong enough drive to breathe on their own.
- Genetic syndromes or anomalies: Some congenital conditions impact the structure or function of the airway.
The decision to place a tracheostomy is made carefully by the medical team, often after consulting with pediatric ENT (ear, nose, and throat) surgeons, pulmonologists, and neonatologists.
What Does Life Look Like After a Tracheostomy?
Babies with tracheostomies may feed, grow, play, and develop like other infants, with some additional care. Many may go home from the NICU once they are stable, even if they still need ventilator support.
Here’s what to expect as you prepare for discharge:
1. Education and Hands-On Training
Before your baby goes home, you’ll receive comprehensive education. This includes:
- How to clean and care for the tracheostomy tube
- How to suction the airway
- What to do if the tube comes out or becomes blocked
- Signs of respiratory distress or infection
- CPR and emergency procedures
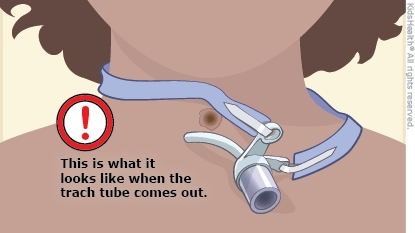
Most hospitals require the infant’s caregivers to demonstrate competence before discharge.
2. Home Nursing and Equipment
Depending on your baby’s needs, home may include:
- A ventilator
- A humidifier to keep the airway moist
- A suction machine to clear secretions
- Spare trach tubes and emergency supplies
Your baby may qualify for home nursing support—either part-time or 24/7 depending on insurance, state guidelines, and medical complexity.
3. Follow-Up Care
After discharge, your baby will continue to be followed closely by:
- Pediatric ENT and pulmonology specialists
- A pediatrician or complex care team
- Physical, occupational, and speech therapists
Some babies may outgrow the need for a tracheostomy and have it removed later in childhood. This process is called decannulation and is done with medical supervision after careful evaluation.
4. Emotional and Community Support
Caring for a child with a tracheostomy is a big responsibility but you are not alone. Many families find comfort in:
- Connecting with other trach families through online or in-person support groups
- Working with a case manager or social worker
- Celebrating milestones—big and small—with your child’s care team
Final Thoughts
While a tracheostomy can seem scary at first, babies with trachs may go on to thrive and grow after discharge. With the right preparation, training, and support, families can become confident, empowered caregivers.
If your baby’s medical team is discussing a tracheostomy, don’t hesitate to ask questions. Your NICU team is there to guide you through each step of the journey.